(UNDATED) – One in four people will have a stroke in their lifetime. After a heart attack or stroke, as many as 1 in 4 survivors will have another one.
Thankfully, 80 percent of strokes can be prevented through healthy lifestyle changes. Sticking to prevention routines – by eating healthy, being active, and taking medications as prescribed – is more important than ever as cases of COVID-19 increase.
During American Stroke Month in May, the American Heart Association encourages people to lead healthier lives to reduce their risk of stroke and heart disease.
A stroke occurs when a blood vessel that carries oxygen and nutrients to the brain is blocked or bursts. This prevents the brain from getting the oxygen and nutrients it needs, causing brain cells to begin dying within minutes. Immediate action is critical with a stroke to reduce the risk of permanent disability or death.
Louisville resident, Mary Ann James, was just 48 when she suffered a stroke. While on a flight home from a trip, Mary Ann developed a headache and intense eye pressure. Once she arrived home, Mary Ann was tired, had trouble focusing, experienced double vision and had problems with coordination. Concerned that something was wrong, Mary Ann’s family took her to urgent care, which directed them to go immediately to the ER. Once there, testing determined that Mary Ann had suffered a massive stroke. Mary Ann stayed in the hospital for 11 days and suffered seizures as a residual effect of her stroke for almost two years.
Today, her seizures are under control and Mary Ann continues to work to improve her health by eating more vegetables, walking as much as she can and laughing often. Of the changes her stroke brought about Mary Ann said, “I decided it was time to take better care of myself. I encourage all women to do the same. So often women focus on their families but pay little attention to their own health. I continue to persevere because I want to be there for my family.”
Secondary prevention and COVID messages
Stroke survivors and people with heart disease may face increased risk for complications if they get COVID-19. Based on current information from the Centers for Disease Control (CDC), it appears people 65 and older and people of any age with underlying medical conditions, such as heart disease, high blood pressure and diabetes are more likely to be infected and to develop more severe symptoms. Stroke survivors may face increased risk for complications if they get COVID-19.
“Treatment for strokes has made amazing progress due to research, clinical advances and healthcare provider education, all impacted by the American Heart Association. COVID has added another challenge, and large vessel strokes in patients less than 50 years old are the prime targets of this devastating type of stroke and the AHA immediately stepped in to educate providers not only about the occurrence but also guidance on prevention and treatment. Without the AHA support, many patients would die. I am proud to support the AHA and will continue to do so because I see results and lives saved by all the AHA does. As a physician, it is so important to have an organization that we can trust, the AHA is that organization. Evidence based high quality care is a mutual goal,” Dr. Kim Perry, Senior Vice President and Chief Medical Officer Kindred Healthcare.
COVID-19 and related strokes
Reports from the front line of the pandemic seem to indicate that some otherwise healthy and younger people with COVID-19 are experiencing strokes and other blood clotting issues.
People of all ages, with or without underlying conditions, should do all they can to stay healthy during this time: washing hands frequently, maintaining social distance, staying home when possible, getting adequate physical activity, eating healthfully. People who have existing conditions such as high blood pressure, diabetes and heart failure must take active steps to manage those conditions with the help of their doctors.
Importance of recognizing warning signs and calling 9-1-1
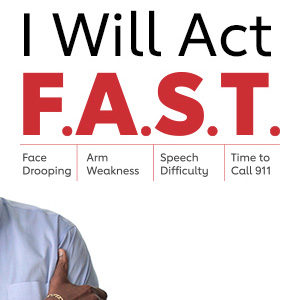
Even as COVID-19 cases strain emergency medicine, calling 9-1-1 is still the best way to access life-saving treatments for people who are experiencing heart attack or stroke symptoms. Emergency medical responders can assess symptoms, begin treatment and transport the patient to the most appropriate hospital, if necessary. The most common stroke symptoms can be remembered using the acronym F.A.S.T. for face drooping, arm weakness or speech difficulty and time to call 9-1-1. Common heart attack symptoms are chest, neck, upper back and jaw pain; shortness of breath; nausea or lightheadedness.
Heart attack and stroke are medical emergencies. If someone is experiencing stroke or heart attack symptoms, they should still call 9-1-1. Emergency medical responders can assess their symptoms, begin treatment in the ambulance, and transport the patient to the most appropriate hospital, if necessary.
- Hospitals have plans in place to keep potentially contagious patients away from others and keep surfaces clean. Calling 9-1-1 and activating Emergency Medical Services (EMS) will ensure that you have the best possible chance to beat a heart attack or stroke. EMS can begin treatment in the ambulance and take you to the hospital best suited to care for you in an emergency.
- As many in the nation face extended time at home, it is possible that heart attack or stroke warning signs may go unnoticed. It is important to check on those who live alone, regularly. Speaking on the phone or video calls can give important clues about common stroke warning signs.
Find more resources to help manage your risk of stroke, visit stroke.org/OneIsEnough.



