
INDIANA— A new report from the American Lung Association (ALA) in Indiana highlights the persistent challenge of lung cancer in the state, revealing that it remains the leading cause of cancer deaths for Hoosiers.
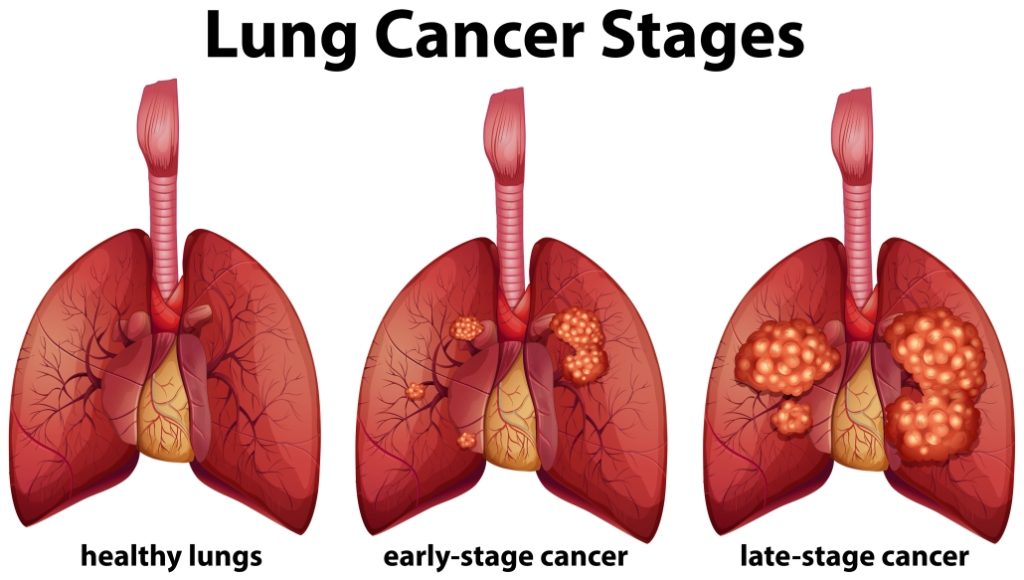
The 2025 “State of Lung Cancer” report reveals that Indiana lags significantly in diagnosing the disease early, a critical factor in improving survival rates.
According to the ALA report, Indiana ranks 39th nationally for early diagnosis, with only 26.8% of lung cancer cases detected at an early, more treatable stage. This figure is slightly below the national early diagnosis rate of 28.1%.

“In the last decade, we have seen incredible progress, including increases in lung cancer survival and early detection rates,” said Tiffany Nichols, director of advocacy for the American Lung Association. “While this progress gives us hope, early detection of lung cancer is far too low in our state. Working to increase awareness and access to lung cancer screening is critical to saving lives.”
The report found that Indiana also struggles with the rate of new cases, ranking 46th nationally with 67.2 new cases per 100,000 people, notably higher than the national rate of 52.8 per 100,000.
Screening and Treatment Access
While Indiana faces challenges in new case rates and early diagnosis, the state is performing better in getting high-risk individuals screened:
- Screening Rate: Indiana ranks 18th nationally for lung cancer screening, with 19.4% of high-risk individuals screened. This is slightly above the national screening rate of 18.2%.
- Biomarker Coverage: Indiana has taken a crucial step in removing financial barriers to advanced care by mandating insurance coverage for comprehensive biomarker testing. This testing examines tumor DNA to determine the most effective treatment options.
The American Lung Association is urging other states across the country to follow Indiana’s lead in requiring insurance coverage for biomarker testing, recognizing it as a crucial policy step to enhance patient outcomes.
The only recommended screening test for lung cancer is the Low-Dose Computed Tomography (LDCT) scan. Major health organizations, including the U.S. Preventive Services Task Force (USPSTF) and the American Cancer Society (ACS), recommend annual LDCT screening for individuals who meet all of the following criteria:
Criteria for High-Risk Lung Cancer Screening
You are considered high-risk and should discuss annual LDCT screening with your healthcare provider if you meet all of these criteria:
- Age: You are between 50 and 80 years old (or 50–77 years old, according to Medicare/CMS guidelines).
- Smoking History: You have a smoking history of at least 20 pack-years.
- A pack-year is defined as smoking an average of one pack of cigarettes (20 cigarettes) per day for one year.
- Current or Recent Smoker Status: You currently smoke or have quit smoking within the last 15 years.
Key Points to Note:
- Asymptomatic: Screening is only for asymptomatic people (meaning they have no signs or symptoms of lung cancer).
- Shared Decision-Making: Before your first LDCT screening, you will need to have a counseling and shared decision-making visit with your doctor. This discussion explores the potential benefits, limitations, and risks of screening, as well as the importance of adhering to annual screening.
- When to Stop Screening: Screening should stop once you turn 81, or if you have developed a severe health problem that limits your life expectancy, or your ability to have lung surgery if cancer is found. Screening should also stop if you have not smoked for 15 years or more.
If you meet these criteria, you are strongly encouraged to contact your doctor to schedule a discussion about annual screening, which can significantly reduce the risk of dying from lung cancer.



